(COPD) Chronic Obstructive Pulmonary Disease
Chronic Obstructive Pulmonary Disease (COPD) is a chronic inflammatory lung disease that causes obstructed airflow from the lungs. It is characterized by long-term breathing problems and poor airflow. The main symptoms include shortness of breath and cough with sputum production. COPD is a progressive disease, meaning it typically worsens over time.
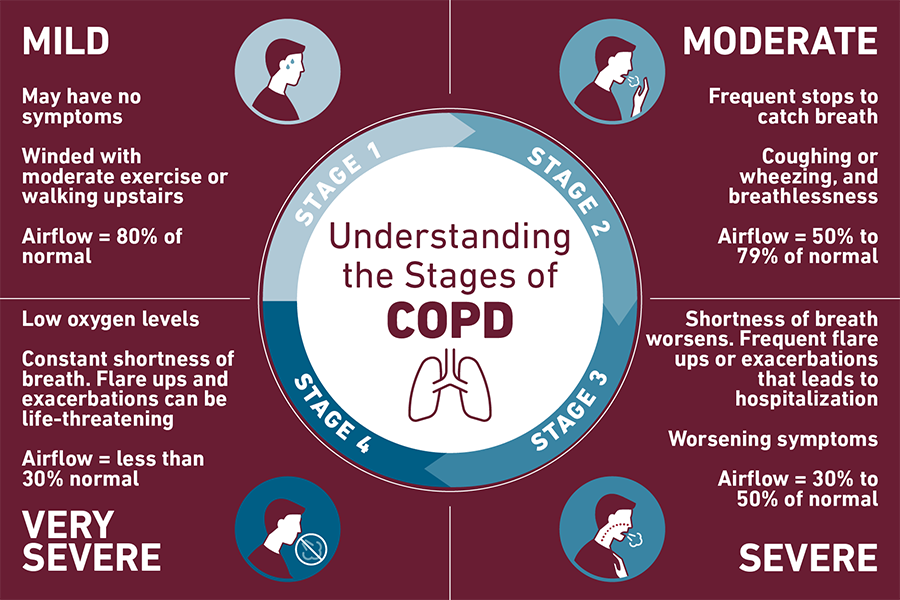
Stages of copd:
Chronic Obstructive Pulmonary Disease (COPD) is classified into different stages based on the severity of airflow limitation. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria is commonly used to stage COPD.
Causes
Chronic Obstructive Pulmonary Disease (COPD) is primarily caused by long-term exposure to substances that irritate and damage the lungs. Here are some of the main causes:
1. Smoking: The most significant risk factor for COPD. Both current and former smokers are at a higher risk.
2. Secondhand Smoke: Exposure to smoke from other people's cigarettes, cigars, or pipes.
3. Air Pollution: Long-term exposure to outdoor air pollution, especially in urban areas.
4 Occupational Hazards: Exposure to dust, chemicals, and fumes in the workplace.
5. Genetic Factors: A rare genetic disorder called Alpha-1 antitrypsin deficiency can cause COPD.
6. Respiratory Infections: Frequent respiratory infections during childhood can increase the risk of developing COPD later in life.
Reducing exposure to these risk factors can help prevent COPD.
Signs and Symptoms
- Shortness of Breath: Especially during physical activities.
- Chronic Cough: Often with mucus (sputum) production.
- Wheezing: A whistling sound when breathing.
- Chest Tightness: Feeling of constriction in the chest.
- Frequent Respiratory Infections: Increased susceptibility to colds, flu, and other respiratory infections.
- Fatigue: Feeling tired or exhausted.
- Unintended Weight Loss: In later stages of the disease.
Additional Symptoms
- Blueness of the Lips or Fingernail Beds (Cyanosis): Due to low oxygen levels in the blood.
- Swelling in Ankles, Feet, or Legs: Due to fluid buildup.
Morning Headaches: Caused by high levels of carbon dioxide in the blood.
These symptoms often develop slowly and may not be noticeable until significant lung damage has occurred.
Pathophysiology of COPD
1. Airway Inflammation: Long-term exposure to irritants like cigarette smoke leads to chronic inflammation in the airways. This inflammation involves various immune cells, including neutrophils, macrophages, and T lymphocytes.
2. Mucus Hypersecretion: The inflammation causes the glands in the airways to produce excess mucus, leading to chronic bronchitis.
3. Airway Remodeling: The chronic inflammation and mucus production cause structural changes in the airways, including thickening of the airway walls and narrowing of the airways.
4. Emphysema: In emphysema, the walls of the alveoli (tiny air sacs in the lungs) are damaged, leading to a loss of elasticity and the collapse of small airways during exhalation. This results in air trapping and hyperinflation of the lungs](https://www.merckmanuals.com/professional/pulmonary-disorders/chronic-obstructive-pulmonary-disease-and-related-disorders/chronic-obstructive-pulmonary-disease-copd).
5. Imbalance of Proteases and Antiproteases: An imbalance between enzymes that break down proteins (proteases) and their inhibitors (antiproteases) leads to the destruction of lung tissue.
6. Oxidative Stress: Increased oxidative stress from inhaled irritants and the body's inflammatory response further damages lung tissue and exacerbates inflammation.
Medications
1. Bronchodilators: These medications help relax the muscles around the airways, making breathing easier. They can be short-acting (for quick relief) or long-acting (for maintenance).
- Short-acting bronchodilators: Albuterol, Ipratropium
- Long-acting bronchodilators: Salmeterol, Tiotropium
2. Inhaled Corticosteroids (ICS): These reduce inflammation in the airways and are often used in combination with bronchodilators.
- Examples: Fluticasone, Budesonide
3. Combination Inhaler: These contain both a bronchodilator and an inhaled corticosteroid.
- Examples: Fluticasone/Salmeterol, Budesonide/Formoterol
4. Phosphodiesterase-4 (PDE4) Inhibitors: These help reduce inflammation and relax the airways.
- Example: Roflumilast
5. Oral Corticosteroids: These are used for short-term treatment during exacerbations.
- Example: Prednisone
6. Antibiotics: These are prescribed during exacerbations if there is a bacterial infection.
Non-Medication Treatments
1. Oxygen Therapy: For patients with severe COPD and low blood oxygen levels, long-term oxygen therapy can improve quality of life and survival.
2. Pulmonary Rehabilitation: A program that includes exercise training, nutritional advice, and education to help manage COPD.
3. Vaccinations: Annual flu shots and pneumococcal vaccines to prevent respiratory infections.
4. Smoking Cessation: The most important step in managing COPD. Quitting smoking can slow the progression of the disease.
Surgical Options
1. Lung Volume Reduction Surgery (LVRS): Removes damaged lung tissue to improve breathing.
2. Bullectomy: Removes large air spaces (bullae) that can interfere with breathing.
3. Lung Transplant: For severe cases, a lung transplant may be considered.
Lifestyle Changes
1. Healthy Diet: Eating a balanced diet to maintain a healthy weight.
2. Regular Exercise: Staying active to improve overall health and lung function.
3. Avoiding Lung Irritants: Reducing exposure to pollutants, dust, and chemicals.
These treatments aim to manage symptoms, prevent complications, and improve the overall quality of life for individuals with COPD -
Nursing Management of copd:
Nursing management of Chronic Obstructive Pulmonary Disease (COPD) involves a comprehensive approach to care that includes assessment, planning, intervention, and evaluation. Here are some key aspects:
Nursing Assessment
- Health History: Assess the patient's smoking history, exposure to pollutants, and family history of respiratory diseases.
- Physical Examination: Observe for signs such as use of accessory muscles, prolonged expiration, barrel chest, and cyanosis.
- Diagnostic Tests: Monitor results of spirometry, chest X-rays, and arterial blood gases.
Nursing Diagnoses
- Ineffective Airway Clearance
- Impaired Gas Exchange
- Activity Intolerance
- Imbalanced Nutrition: Less than Body Requirements
- Risk for Infection
Nursing Interventions
1. Airway Management: Encourage effective coughing techniques and use of suctioning if necessary.
2. Breathing Exercises: Teach pursed-lip breathing and diaphragmatic breathing to improve ventilation.
3. Oxygen Therapy: Administer oxygen as prescribed and monitor oxygen saturation levels.
4. Medication Administration: Administer bronchodilators, corticosteroids, and other medications as prescribed.
5. Nutritional Support: Provide small, frequent meals that are high in calories and protein to prevent weight loss.
6. Hydration: Encourage adequate fluid intake to thin mucus secretions.
7. Patient Education: Educate the patient about smoking cessation, medication adherence, and avoiding respiratory irritants.
8. Pulmonary Rehabilitation: Encourage participation in pulmonary rehabilitation programs to improve physical conditioning.
9. Infection Prevention: Promote hand hygiene, vaccination, and avoidance of crowds during flu season.
Evaluation
- Monitor the patient's respiratory status and response to interventions.
- Assess for improvement in symptoms such as dyspnea, cough, and fatigue.
- Evaluate the patient's ability to perform activities of daily living.
- Assess for improvement in symptoms such as dyspnea, cough, and fatigue.
- Evaluate the patient's ability to perform activities of daily living.
No comments:
Post a Comment